Computational modeling of heart valves
The human heart has four chambers, separated by heart valves, whose task it is to ensure unidirectional blood flow. The mitral valve (MV) regulates the blood flow between the left atria and the left ventricle and pathologies of the MV entail a significant impact on patient mortality and morbidity. To treat a diseased mitral valve, the valve is repaired using either surgical techniques via open heart surgery or interventional techniques. Both valve repair strategies put the patient at risk, thus, a successful valve repair outcome is essential. Additionally, congenital heart disease in pediatrics is often complex, as anatomical anomalies that arise during pregnancy often entail a high variance on a patient-to-patient level, making valve repair planning challenging.
Our research aims to develop simulation models of heart valve diseases. These can provide valuable insight into the valve dynamics prior or/and after surgery and may thus aid clinicians in the choice of treatment strategy. By virtually testing different valve repair options in a simulation model, a well-informed decision on the valve repair method can be made thus increasing the possibility of a positive valve repair outcome and improving patient-specific care. Using fluid-structure interaction (FSI), which combines computational fluid dynamics and finite element modeling, the heart valve leaflets and the blood flow are modeled, Fig. 1.
Currently, the development of patient-specific models using healthy adult volunteers is ongoing. This is the first step toward models of children with heart disease, to ensure a properly working model that produces results that coincide well with ultrasound data.
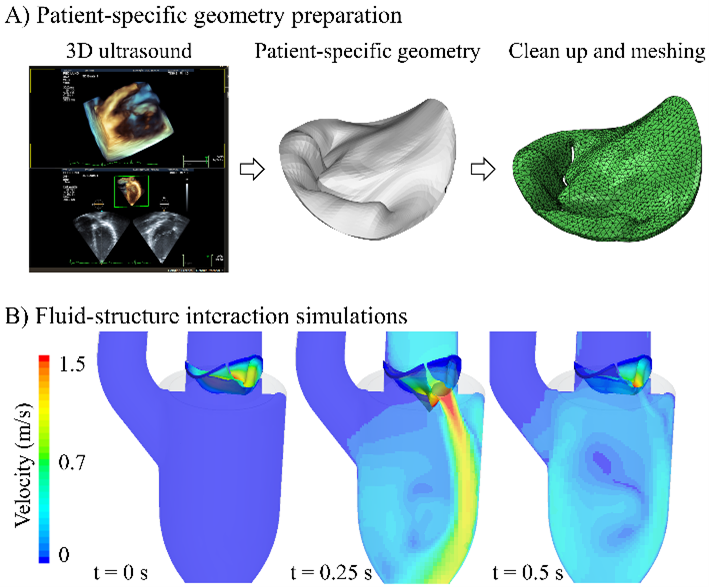
Figure 1: Patient-specific heart models using fluid-structure interaction. A) The patient-specific heart valve is digitalized using 3D ultrasound images, after which it is meshed and then inserted into the simulation model. B) Preliminary results on the first patient-specific simulations, showing the velocity distribution in a cross-sectional plane during the opening of the valve.
Researchers at BME: PhD student: Lea Christierson; Supervisor: Hanna Isaksson
Collaborators at LU: PI: Nina Hakacova (Department of Clinical Sciences); Supervisors: Johan Revstedt (Department of Energy Science), Petru Liuba (Department of Clinical Sciences)
Funding: The pediatric heart foundation and the Heart-lung foundation
